Hysterectomies, a critical surgical procedure often required for gynecologic cancers and other health conditions, stand as the second most common operation among women of reproductive age in the United States, with over 600,000 performed annually. While some pain post-surgery is expected, experiencing prolonged sore hips after hysterectomy, which could point towards issues like nerve damage or scar tissue formation, is not an anticipated part of the recovery process.
This guide aims to address the complex issue of managing sore hips after hysterectomy, with an emphasis on understanding the causes of hip pain, such as joint inflammation or muscle spasms, and providing strategies for effective pain relief. These may include physical therapy options designed for post-surgical recovery or massage therapy to alleviate chronic pain in the pelvic area, ensuring that individuals can navigate their path to healing with confidence.
Understanding Hip Pain After Hysterectomy
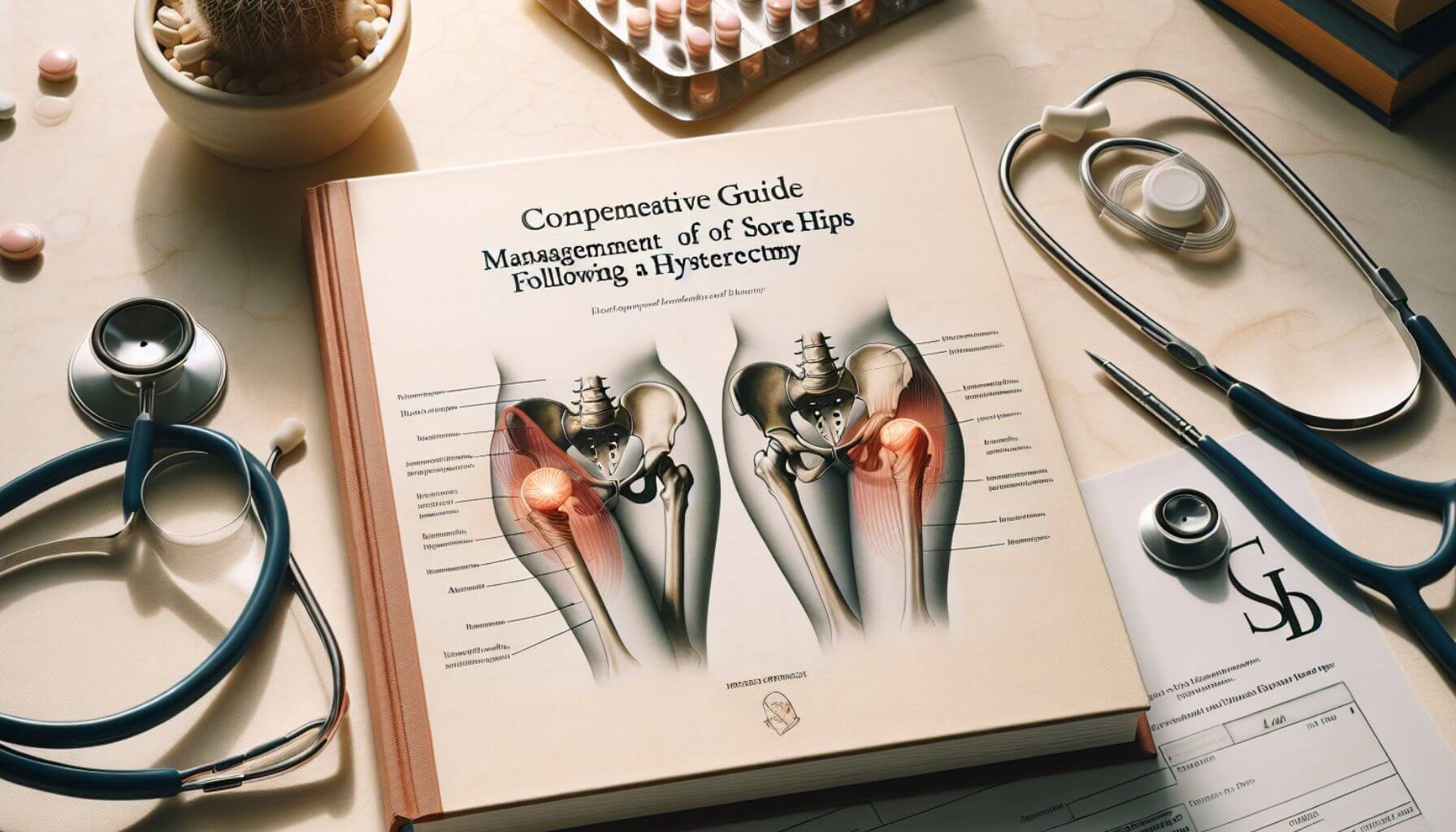
Causes and Mechanisms of Hip Pain Post-Hysterectomy
Hysterectomy procedures can disrupt the normal anatomy and function of the pelvic region, leading to various forms of discomfort and pain. One common issue is the formation of adhesions, which are bands of scar tissue that can cause organs and tissues to stick together, potentially leading to long-term pain [Webpage 2]. Additionally, the surgical procedure often requires positioning that may strain the hip joints. Specifically, the dorsal lithotomy position used during surgery can place significant stress on the hip joints, contributing to postoperative hip pain.
Evaluating and Understanding Pain Symptoms
To assess the severity and nature of hip pain following a hysterectomy, medical professionals may utilize several diagnostic tools. The Visual Analog Scale (VAS) and the Douleur Neuropathique 4-questionnaire (DN-4) are commonly used to evaluate pain symptoms, helping to distinguish between general and neuropathic pain types [Webpage 3]. Additionally, the abdominal pressure threshold can be measured using an algometry device, and sensorial alterations may be assessed with a Von Frey Filament to understand the extent of nerve involvement or damage [Webpage 3].
Contributing Factors to Persistent Hip Pain
Several factors can contribute to the persistence of hip pain after hysterectomy. These include underlying pelvic floor muscle spasms, which not only cause pain directly but also lead to pelvic girdle weakness. This weakness can result in the overuse of surrounding hip muscles, exacerbating discomfort. Furthermore, nerve damage during surgery is a significant cause of hip pain, with symptoms ranging from mild discomfort to severe pain, often accompanied by numbness or tingling sensations in the affected areas. Joint inflammation, another potential post-surgical complication, can arise from surgical trauma, infection, or an immune response, adding another layer of complexity to the management of post-hysterectomy hip pain.
Preventing Hip Pain After Surgery
Establishing a Baseline Analgesic Regimen
To mitigate hip pain after a hysterectomy, it’s essential to establish a baseline analgesic regimen. This should ideally include acetaminophen, an NSAID, dexamethasone, and opioids as rescue analgesics. Such a regimen addresses pain from multiple angles, reducing inflammation and managing acute pain episodes effectively.
Home and Lifestyle Adjustments
- Home Preparation: Rearrange your living space to ensure necessities are within easy reach, ideally at waist level. Incorporate aids like a perching stool to minimize strain during daily tasks.
- Recovery and Mobility: Balance rest with gentle activities. Start with short walks and gradually include supervised physiotherapy or hydrotherapy to enhance recovery without overstraining the hips.
- Nutritional Considerations: Focus on a balanced diet rich in proteins, vitamins, and minerals to support the healing process and strengthen the body’s recovery capacity.
Mindful Recovery Practices
Being mindful of your physical activities and personal habits is crucial. For instance, avoid sexual activities for the first six weeks post-surgery to prevent hip strain. When resuming, be cautious of hip positioning to avoid further complications. Additionally, modify travel plans to prevent prolonged sitting, which can increase the risk of Deep Vein Thrombosis (DVT).
Effective Management and Relief Strategies
Physical Therapy and Non-Surgical Approaches
Clear Passage Physical Therapy, renowned for its expertise in non-surgical treatments, addresses pelvic pain and adhesions effectively, with over three decades of experience focusing on post-hysterectomy recovery [Webpage 2]. Their approach includes the PRM Protocol™, which integrates physical therapy with nutritional guidance and behavioral health to manage sore hips effectively. For those experiencing severe adhesion issues, treatments can reduce symptoms like low back pain and discomfort during intercourse significantly.
Pain Management Techniques
A comprehensive pain management strategy is crucial for alleviating hip pain after a hysterectomy. Options include a combination of physical therapy, which has been shown to significantly decrease adhesion-related pelvic pain [Webpage 2], and chiropractic care to address pain due to ligamentous rearrangement and surgical positioning. Additionally, pharmacological approaches such as Celecoxib help manage pain effectively due to its properties like rapid absorption and selective COX-2 inhibition. For immediate postoperative pain relief, techniques such as intra-articular injections with a cocktail of ropivacaine, ketorolac, and morphine have proven effective.
Post-Operative Care and Recommendations
Post-surgery, it is essential to adhere to specific care instructions to mitigate pain and accelerate recovery. This includes managing pain with prescribed medications—being cautious not to exceed recommended doses to prevent liver damage—and following dietary recommendations to avoid constipation and promote healing. Physical mobility should be gradually reintroduced, adhering to guidelines on the use of mobility aids and the timing for resuming activities like driving and sports. Keeping the surgical site clean and monitoring for any signs of infection are also paramount to ensure a smooth recovery.
When to Seek Further Medical Assistance
Recognizing Serious Symptoms
- Persistent or Severe Pain: If pain in the hips persists beyond three months post-surgery or worsens significantly, it’s crucial to consult a pelvic pain specialist.
- Complications Indicative of Infections: Symptoms such as vaginal discharge with a foul odor, signs of a urinary tract infection (UTI), or an incision infection characterized by prolonged constipation, diarrhea, fever, nausea, or vomiting necessitate immediate medical consultation.
- Symptoms of Deep Vein Thrombosis (DVT) or Pulmonary Embolism: Experiencing severe swelling, redness, difficulty walking, or symptoms indicative of a pulmonary embolism, such as sudden shortness of breath, are emergencies requiring urgent care.
Diagnostic and Treatment Options
- Initial Consultation and Examinations: During the first medical visit post-symptoms, expect a comprehensive review of your medical history, along with external and internal examinations. Imaging tests such as ultrasounds, CT scans, or MRIs might be conducted to identify any abnormal growths or structures causing pain.
- Lab Tests and Laparoscopy: Blood and urine tests will check for underlying conditions that could be causing pelvic pain. Additionally, a laparoscopy might be performed to look for abnormal tissues or infections in the pelvic organs.
- Available Treatments: Depending on the diagnosis, treatments may include pain relievers, hormone treatments, antibiotics, antidepressants, muscle relaxers, physical therapy, spinal cord stimulation, trigger point injections, or psychotherapy.
Monitoring and Managing Chronic Pain
- Ongoing Evaluation: If chronic pain persists after six months, despite previous consultations with healthcare providers, consider seeking a specialist in nerve injuries or disorders. This step is crucial as persistent pain may be related to nerve damage.
- Daily Pain Management: It is essential to monitor the intensity and duration of hip pain daily. If pain interferes significantly with daily activities or does not improve with standard treatments, further evaluation by your healthcare provider is recommended to adjust the treatment plan appropriately.
Conclusion
Through comprehensive evaluation and management strategies, individuals facing sore hips after a hysterectomy can find routes to significant relief and healing. The causes, ranging from surgical positioning to nerve damage and joint inflammation, necessitate a multidimensional approach to care. Implementing a baseline analgesic regimen, making thoughtful home and lifestyle adjustments, and engaging in physical therapy and non-surgical treatments have been underscored as pivotal in navigating the path to recovery. These concerted efforts equip patients with the necessary tools to manage pain effectively and mitigate the impact of surgery on their daily lives.
The significance of recognizing persistent pain and seeking timely medical assistance cannot be overstated, as it could denote complications requiring specialized care. Further diagnostic evaluations and tailored treatment plans play a critical role in addressing the underlying causes of post-hysterectomy hip pain. Ultimately, by adhering to the recommended post-operative care, actively participating in recovery practices, and being attuned to their bodies’ signals, individuals can optimize their healing process and improve their quality of life post-surgery. This guide aims to empower patients with knowledge and strategies to manage sore hips after a hysterectomy, emphasizing the importance of self-care and professional guidance on their journey to recovery.
FAQs
- Why am I experiencing severe hip pain after my hysterectomy?
The hip pain you’re experiencing after a hysterectomy is likely due to the positioning during surgery, known as the dorsal lithotomy position, which can place considerable stress on the hip joints. - What can I do to alleviate joint pain following a hysterectomy?
Post-hysterectomy recovery varies for each individual and can be challenging. Joint pain, particularly in the morning, may indicate a need for reconditioning. Incorporating gentle stretching and daily activities like brisk walking can enhance joint mobility and reduce discomfort. - How can I strengthen my pelvic muscles post-hysterectomy?
To strengthen your pelvic muscles after a hysterectomy, try performing pelvic tilts: Lie on your back with your knees bent, draw in your lower abdominal muscles, and gently squeeze your pelvic floor and buttocks. Tilt your pelvis upwards, pressing your back flat against the bed. Hold this position for up to 10 seconds and then relax. Repeat this exercise up to 10 times. - Why are my legs extremely painful after a hysterectomy?
The pain in your legs after a hysterectomy could be due to reduced blood circulation, which heightens the risk of developing deep vein thrombosis (DVT) in your legs. Engaging in simple calf muscle exercises can help improve circulation in your lower legs during recovery.
[1] – https://pelvicrehabilitation.com/symptoms/pain-after-hysterectomy/
[2] – https://www.bwclinic.com/blog/2021/11/25/chiropractic-for-hip-pain-after-a-hysterectomy
[3] – https://pelvicfloorpro.com/hip-pain-after-pelvic-surgery/
[4] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5370797/
[5] – https://rapm.bmj.com/content/44/4/425
[6] – https://www.kingedwardvii.co.uk/health-hub/hip-replacement-recovery-tips
[7] – https://clearpassage.com/pain-after-surgery/hysterectomy-pain/
[8] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6942092/
[9] – https://www.allinahealth.org/health-conditions-and-treatments/health-library/patient-education/preparing-for-your-hysterectomy/the-day-of-your-surgery/how-to-manage-your-pain-after-surgery
[10] – https://orthoinfo.aaos.org/en/recovery/activities-after-hip-replacement/
[11] – https://www.healthline.com/health/womens-health/signs-of-overdoing-it-after-hysterectomy
[12] – https://www.baltimoreperipheralnervepain.com/blog/causes-of-chronic-pain-following-surgery-in-the-pelvic-area.cfm
[13] – https://www.hystersisters.com/vb2/showthread.php?t=466388
[14] – https://www.mayoclinic.org/diseases-conditions/chronic-pelvic-pain/diagnosis-treatment/drc-20354371
[15] – https://www.spirehealthcare.com/health-hub/specialties/womens-health/hysterectomy-recovery-timeline-and-tips/